Purity 98 % (TLC)
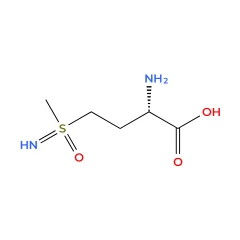
Name: L-Methionine sulfoximine
Synonyms: L-S-(3-Amino-3-carboxypropyl)-S-methylsulfoximine, L-Methionin-S R-sulfoximine, L-Methionine sulfoximine, Cas 15985-39-4, 15985-39-4, inhibitor of glutamine synthetase, glutamine synthetase inhibitor
Cas No: 15985-39-4
Chemical Formula C5H12N2O3S
Molecular Weight 180.23
Appearance white solid
Storage temperature Room temperature
L-Methionine-DL-sulfoximine (MSX; MSO), a highly specific and irreversible inhibitor of Glutamine synthetase (GS), is also a potent convulsant which metabolically and morphologically primarily affects astroglia. L-Methionine-DL-sulfoximine has been employed to inhibit the Gln-dependent ammonia-stimulated neuronal toxicity in vitro, potentiating Gln deficit-dependent depression. L-Methionine-DL-sulfoximine tremendously increases the rate of release of fixed nitrogen in cyanobacteria. L-Methionine-DL-sulfoximine is a promising candidate for research in biofertilizers and convulsive seizures (CS).
| Cat nr | Stock | Quantity (gr) | Price |
| 81307030005 | In stock | 5 g | €525 |
| 81307030010 | In stock | 10 g | €875 |
| 81307030050 | In stock | 50 g | €2550 |
| 81307030100 | In stock | 100 g | €3850 |
**Pricing disclaimer
Methionine sulfoximine (MSO) is a compound originally discovered as a byproduct of agene-based milled flour maturation. MSO irreversibly inhibits the astrocytic enzyme glutamine synthase (GS) but also interferes with the transport of glutamine (Gln) and of glutamate (Glu), and γ-aminobutyric acid (GABA) synthesized within the Glu/Gln-GABA cycle, in this way dysregulating neurotransmission balance in favor of excitation.
Albrecht, J., Czuczwar, S.J., Zielińska, M. et al. Methionine Sulfoximine as a Tool for Studying Temporal Lobe Epilepsy: Initiator, Developer, Attenuator. Neurochem Res 50, 84 (2025). https://doi.org/10.1007/s11064-024-04329-z
L-Methionine sulfoximine (MSX) is a powerful inhibitor of glutamine synthetase activity, widely used as a selection agent for plasmid integration in Chinese hamster ovary (CHO) and other mammalian cell lines. The increasing demand for high-yield cell banks for recombinant protein production in therapeutics has led to the development of two primary selection systems for stable and active clones: Methotrexate (MTX) selection, which targets dihydrofolate reductase (DHFR) overexpression, and MSX selection, which enhances glutamine synthetase (GS) expression.
In the MSX-based system, cells are cultured in glutamine-free media, and inhibition of endogenous glutamine synthetase activity leads to cell death in those lacking overexpression. Compared to the Methotrexate-DHFR system, MSX-GS selection offers distinct advantages, including a single amplification step and a significantly shorter timeline for generating high-stability, highly amplified clones.
Beyond its role in cell selection, MSX influences various biological pathways. It has been shown to increase ornithine decarboxylase activity, reduce cell survival in transient cerebral ischemia models, and strongly inhibit glutamine synthetase activity. These effects make MSX a valuable tool in biochemical and neurological research, particularly in studies exploring amino acid metabolism and cellular stress responses.
Dandan Wang et al (2024)
nvestigated the impact of glutamine synthetase (GS) inhibition on glioma vascular permeability and its underlying mechanism. Using C6 glioma rat models, researchers divided the subjects into a control group and an L-methionine sulfoximine (MSO) treatment group, administering MSO intraperitoneally every other day for a total of three doses. Tumor vascular permeability was assessed through tail vein injection of Evans blue dye, while GS activity, glutamate, glutamine, and arginine concentrations were measured. Further analysis included qPCR experiments to examine the effect of glutamate on N-methyl-D-aspartate (NMDA) receptor expression, along with nitric oxide synthase (NOS) and nitric oxide (NO) assays to assess changes in NOS activity and NO levels.
The results showed that MSO increased glioma vascular permeability by inhibiting GS activity, leading to elevated glutamate levels. This increase in glutamate activated NMDA receptors, which in turn stimulated NOS activity and led to a rise in NO production. Higher NO levels, along with increased arginine and NOS activity, contributed to enhanced vascular permeability due to the vasodilatory effects of NO.
In conclusion, inhibiting GS in gliomas leads to increased vascular permeability, primarily through NO-mediated vasodilation. These findings suggest that GS may be a key target for regulating glioma blood flow and could have implications for improving therapeutic delivery and treatment outcomes.
Dandan Wang et al.; Anticancer Research November 2024, 44 (11) 4869-4875; DOI: https://doi.org/10.21873/anticanres.17312